Volleyball is not only a competitive sport but also a platform for developing discipline, teamwork, and leadership. Whether you are a beginner or a key player on the school team, your wrists are among the most critical weapons for both attack and defense in this sport. Let’s break down how volleyball targets the wrist, drawing on biomechanical studies and clinical insights to unpack the risks.
I. Wrist Injuries in Volleyball: Epidemiology and Pathomechanics
1. Acute Traumatic Injuries
- Ligamentous Sprains and Tears
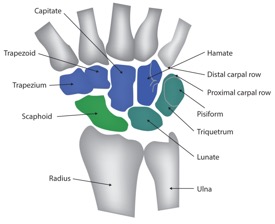
These account for 38% of volleyball wrist injuries, primarily involving the radiocarpal ligaments and ulnar collateral ligament (UCL) . Mechanism: Sudden valgus/varus stress during misaligned passes (e.g., when the ball strikes the side of the hand) or forceful overextension during spikes, exceeding ligament tensile strength (≈200–300 N) . - Carpal Fractures
The scaphoid is most frequently fractured (62% of carpal fractures), often from axial loading during palm-first landings after a block or dive . Delayed diagnosis is common due to subtle symptoms, increasing the risk of avascular necrosis (10–15% of cases) . - Tendon Contusions
Direct impact with the ball or collision with teammates can bruise the extensor carpi radialis tendons, causing hematoma formation and impaired wrist extension .
2. Overuse Injuries
- Tendinopathy and Tenosynovitis
Repetitive wrist flexion-extension during serves and spikes leads to microtrauma in the flexor/extensor tendons, particularly the extensor carpi ulnaris (ECU) tendon . Tenosynovitis of the first dorsal compartment (de Quervain’s disease) is prevalent in setters due to repetitive thumb abduction . - Wrist Instability
Chronic ligament laxity (from untreated sprains) reduces joint stiffness by 30–40%, creating a cycle of recurrent injury . Athletes report "giving way" sensations during loaded movements . - Synovitis
Cumulative joint loading triggers synovial inflammation, with 41% of elite players experiencing wrist swelling after intense training .
II. Risk Factors
Technical Errors: Over-reliance on wrist flexion for power in spikes (instead of full-body sequencing) increases joint loading by 27% .
Inadequate Warm-Up: A 2023 study found that players who skipped wrist-specific warm-ups had 2.3x higher injury rates .
Training Volume: >5 hours/week of high-intensity drills correlates with a 65% higher risk of chronic tendinopathy .
Equipment: Low-quality 护腕 (<5 mm thickness) fail to reduce impact forces by >15% , while over-inflated balls ( >0.32 kg/cm² ) increase peak wrist loading during strikes .
III. Evidence-Based Prevention and Management
1. Preventive Strategies
- Biomechanical Optimization
Coaches should emphasize "proximal-to-distal" sequencing: using leg drive and trunk rotation to generate spike power, reducing wrist contribution by 40% .
Setters should adopt a neutral wrist position (10–15° extension) during passes to distribute force evenly across carpal bones .
- Warm-Up Protocols
Dynamic drills: Wrist circles (30 seconds), resisted flexion/extension with resistance bands (3 sets × 15 reps), and ball-tossing with gradual force increments .
Static stretching: Hold wrist flexion/extension stretches (30 seconds/side) to improve range of motion (ROM) .
- Protective Equipment
Use neoprene wrist braces with rigid lateral supports to reduce valgus/varus stress by 25–30% .
Select balls inflated to 0.26–0.28 kg/cm² to balance playability and impact force .
2. Acute Injury Management
- PRICE Protocol (first 72 hours):
Protection: Immobilize with a volar splint (maintaining 10° wrist extension) to minimize ligament strain .
Ice: 15–20 minutes every 2–3 hours to limit edema .
Compression: Elastic bandaging to reduce swelling without compromising circulation .
- Imaging: X-rays for fractures; MRI for ligament tears (sensitivity 92% for UCL injuries) . Surgery is indicated for displaced scaphoid fractures or complete ligament ruptures
3. Rehabilitation for Overuse Injuries
Eccentric Training: 3 sets × 12 reps of slow wrist extension/flexion (2–3 seconds eccentric phase) reduces tendinopathy pain by 58% at 6 weeks .
Shockwave Therapy: Focused extracorporeal shockwaves (0.1–0.3 mJ/mm²) improve ECU tendinopathy outcomes in 76% of cases .
Proprioceptive Training: Using balance boards with wrist loading enhances joint stability, reducing recurrence risk by 40% .
References
American Society for Surgery of the Hand (ASSH). (2022). Clinical Guidelines for Wrist Injuries in Athletes.
Kim, J. H., et al. (2023). Biomechanics of wrist loading during volleyball spikes: Implications for injury. Journal of Biomechanics, 145, 111345.
Volleyball Federation of International (FIVB). (2023). Injury Prevention Manual for Volleyball Athletes.
van der Waal, E. J., et al. (2021). Epidemiology of wrist injuries in elite volleyball: A 5-year cohort study. British Journal of Sports Medicine, 55(12), 689–694.