{{expert.day}}
{{expert.month}}
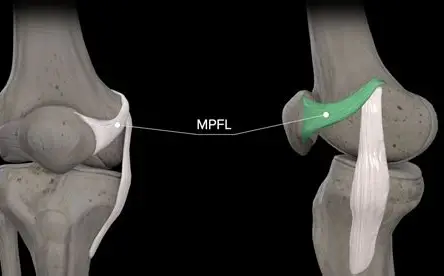
Recurrent patellar dislocation is a common orthopedic issue in skeletally immature patients, particularly adolescents engaged in sports requiring cutting and pivoting motions. The medial patellofemoral ligament (MPFL) serves as the primary passive stabilizer against lateral patellar displacement. Traditional MPFL reconstruction techniques risk physeal damage in growing children, potentially causing growth disturbances. The growth-sparing MPFL reconstruction technique has emerged as a safe and effective solution, preserving the distal femoral and proximal tibial physes while restoring patellar stability.
Anatomical Considerations in Pediatric Patients
MPFL Anatomy:
1 Originates between the adductor tubercle and medial femoral epicondyle
2 Inserts on the superomedial patella
3 Provides 50-60% of restraining force against lateral patellar displacement
Growth Plate Vulnerabilities:
1 Distal femoral physis: Contributes to 70% of femoral growth
2 Proximal tibial physis: Critical for tibial length development
3 Traditional femoral tunnel drilling risks premature physeal closure and limb length discrepancy
Growth-Sparing Surgical Techniques
1. Physeal-Avoiding Femoral Fixation
·(1)Epiphyseal or Metaphyseal Graft Fixation:
*Femoral attachment positioned distal to physis using fluoroscopic guidance
*Fixation with suture anchors or interference screws in safe zones
(2)Adductor Magnus Tenodesis (AMT):
*Utilizes adductor magnus tendon as an autologous stabilizer
*Avoids femoral drilling entirely
2. Soft Tissue Graft Options
(1)Gracilis or Semitendinosus Autograft (most common)
(2)Quadriceps Tendon Autograft (preserves hamstrings)
(3)Allograft (reduces donor-site morbidity)
3. Physeal-Sparing Patellar Fixation
(1)Suture Anchor Technique:
*Anchors placed in superomedial patellar border
*Avoids transosseous tunnels near the proximal tibial physis
(2)Soft Tissue Weave:
*Graft woven through medial patellofemoral soft tissues
Clinical Outcomes
1 Success Rates
(1)90-95% stability restoration in pediatric cohorts (Nietosvaara et al., 2022)
(2)Recurrence rates <5% vs. 15-20% with non-operative management
2 Growth Preservation
(1)No reported growth disturbances in physeal-sparing techniques (Parikh et al., 2023)
(2)Limb length symmetry maintained at skeletal maturity
3 Rehabilitation Protocol
(1)Phase 1 (0-6 weeks):
*Knee immobilizer with protected weight-bearing
*Quadriceps activation and straight leg raises
(2)Phase 2 (6-12 weeks):
*Progressive ROM (0°-90° by week 8)
*Closed-chain strengthening (mini-squats, step-ups)
*Phase 3 (3-6 months):
*Sport-specific agility drills
*Isokinetic strength testing for clearance
(3)Return to Sport (6-9 months):
*Requires >90% quadriceps symmetry and no apprehension
Growth-sparing MPFL reconstruction provides excellent patellar stability while preserving physeal integrity in skeletally immature patients. With proper surgical technique and rehabilitation, young athletes can return to sports safely with minimal risk of recurrence or growth complications.
References
Nietosvaara Y, et al. (2022). Growth-Sparing MPFL Reconstruction in Children. J Pediatr Orthop.
Parikh SN, et al.(2023). Physeal-Sparing Techniques for Patellar Instability. Am J Sports Med.